The Obama Administration made a surprise announcement yesterday that implementation of the new employer and insurer reporting requirements under the Affordable Care Act (ACA) has been postponed. Planned to commence on January 1, 2014, implementation of the large employer penalty and related employer mandate have been pushed back one year. This means that employers and/or employer groups with 50 or more full-time employees now have until January 1, 2015, to offer health insurance to their full-time employees.
According to a statement released by the Treasury Department, the postponement is in response to employers’ concerns about the complexity of the reporting requirements and the need for more time to implement them effectively.
“This is designed to meet two goals,” said Mark J. Mazur, Assistant Secretary for Tax Policy, U.S. Department of the Treasury. “First, it will allow us to consider ways to simplify the new reporting requirements consistent with the law. Second, it will provide time to adapt health coverage and reporting systems while employers are moving toward making health coverage affordable and accessible for their employees.”
Postponement of “Pay or Play” Employer Shared Responsibility Payments (Under Section 4980H)
Beginning January 1, 2014, large employers that did not offer health insurance coverage were to pay a penalty of $2,000 per employee, and those offering unaffordable coverage were to pay a $3,000 per employee penalty for those employees who purchased coverage on an exchange and received a Federal subsidy. Because it will be impractical to determine which employers owe shared responsibility payments (under section 4980H) during the transition, these employer penalties will not apply until 2015.
Information Reporting (Under Sections 6055 and 6056)
Proposed rules are expected to be published this summer regarding information reporting (under sections 6055 and 6056). Once the final rules are issued, employers, insurers and other reporting entities will be strongly encouraged to voluntarily implement this information reporting in 2014 as a “field test” in advance of full implementation in 2015.
Other Areas of ACA Not Affected
No other provision of the ACA is affected by this announcement, including the individual mandate that every American have health insurance or pay a penalty; the required establishment of exchanges where individuals can purchase health coverage plans; and employees’ access to the premium tax credits available under the ACA.
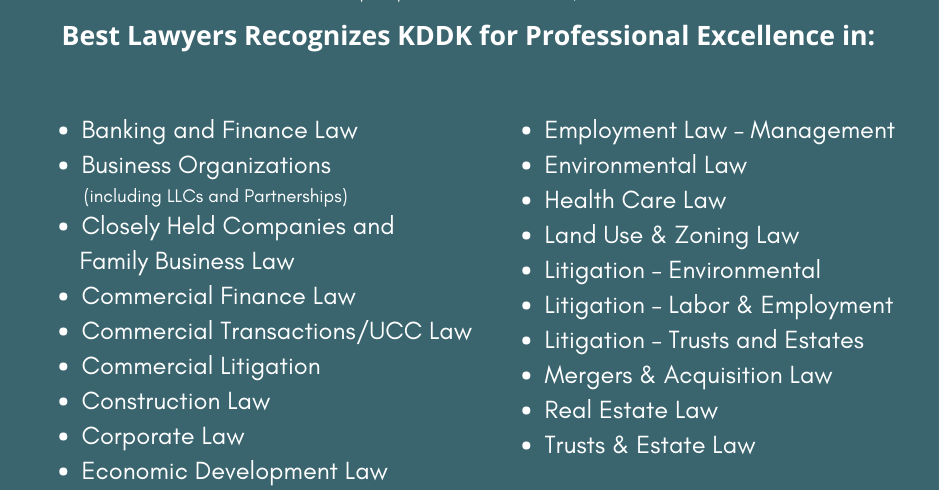
For more information about the ACA or any related area of law, please contact Mark Samila at MSamila@KDDK.com, Steve Theising at STheising@KDDK.com or Ashley Bess at ABess@KDDK.com; or call (812) 423-3183 to speak to any member of the KDDK Tax and Employee Benefits Law Practice Team.
About the Author

Ashley R. Bess, an attorney at Kahn, Dees, Donovan & Kahn, LLP, in Evansville, Indiana, practices in the areas of business law, contract negotiation and creditors’ rights and collections. Ashley earned her B.S. in political science magna cum laude from the University of Evansville, and her J.D. magna cum laude from Valparaiso University School of Law.